Obesity is a global health issue that continues to rise, and Spain is no exception. According to the Spanish Society for the Study of Obesity (Seedo), 21% of Spanish adults suffer from obesity, and 40% are overweight. Additionally, a concerning 18% of the child and adolescent population is also affected by obesity. These figures are alarming, and if no action is taken, it is projected that by 2034, 37% of the adult population in Spain will suffer from obesity, according to estimates from the “World Obesity Atlas”.
Obesity and overweight are more than just aesthetic issues; they significantly increase the risk of developing various types of cancer, though the exact reason for this relationship is not entirely clear. In fact, it has not been established whether obesity is the direct cause of the increased cancer risk.
A) Obesity: More Than Just Fat Accumulation
Obesity is not just about excess adipose tissue; it is a disease that affects the entire body. Fat tissue damaged by weight gain can disrupt the functioning of nearly all organs. Research suggests that obesity may originate from physical alterations that in turn cause changes in the body, or vice versa.

B) Cancer and Obesity: A Comprehensive Scientific Analysis
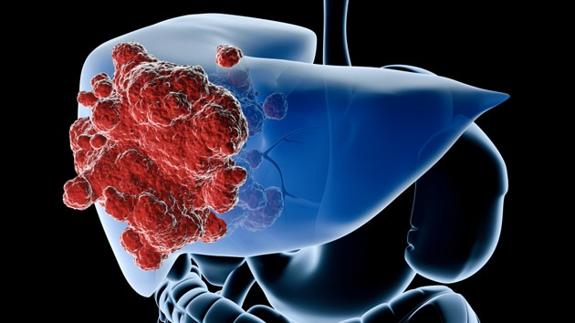
The Organ Interaction in Metabolic Diseases Group at CNIO, led by Guadalupe Sabio, studies how obesity is related to cancer. Guadalupe explains that epidemiological studies show a high correlation between obesity and certain types of cancer, particularly liver and colon cancer. These studies began in 2010, and since then, the relationship has been confirmed in animal models.
Guadalupe’s group has identified certain proteins in adipose tissue that are more active in obese individuals. These proteins appear to be related to an increased risk of cancer, and when they were eliminated in animal models, the risk of developing liver cancer decreased. Interestingly, women seem to have this pathway less active than men, which might explain why men are four times more likely to develop liver cancer.
C) Pancreatic Cancer, Obesity, and the Microbiome
Núria Malats, who leads the Epidemiology and Molecular Genetics Group at CNIO, has investigated the relationship between obesity and pancreatic cancer. Although obesity is known to be a risk factor, the exact relationship is complex and may be mediated by type 2 diabetes, which also increases the risk of pancreatic cancer. Additionally, chronic and mild inflammation of the pancreas, which could be related to the microbiome, is another possible cause of this disease.
D) Metastasis and Obesity
Héctor Peinado, head of the Microenvironment and Metastasis Group at CNIO, focuses on how obesity influences the spread of cancer in the body. His research suggests that obesity increases vascular permeability and platelet activity, which facilitates the formation of metastases. Peinado is working on strategies to reverse these effects, such as dietary changes and the use of platelet aggregation inhibitors.
E) Relationship Between Obesity and Cancer
Understanding how obesity and overweight contribute to the development of cancer is crucial for modern oncology. Between 2011 and 2015, in the United States, 37,670 new cancer cases in men and 74,690 in women were linked to excess body weight. Moreover, in that country, most obesity-related cancers increased by 7% between 2005 and 2014, while cancers related to other factors decreased by 13%.
There are thirteen types of cancer whose risk is significantly increased by obesity or overweight. These include endometrial cancer, esophageal adenocarcinoma, gastric cancer, liver cancer, kidney cancer, multiple myeloma, meningioma, pancreatic cancer, colorectal cancer, gallbladder cancer, breast cancer, and thyroid cancer. Notably, each 5-unit increase in Body Mass Index (BMI) raises the risk of breast and ovarian cancer after menopause.
Conclusion
The relationship between obesity, overweight, and cancer is complex and multifaceted. Advancing our understanding of this connection is essential to developing prevention and treatment strategies that can reduce cancer incidence in a population increasingly affected by obesity. Research in this field remains crucial to offering new hope to those battling this disease.






























